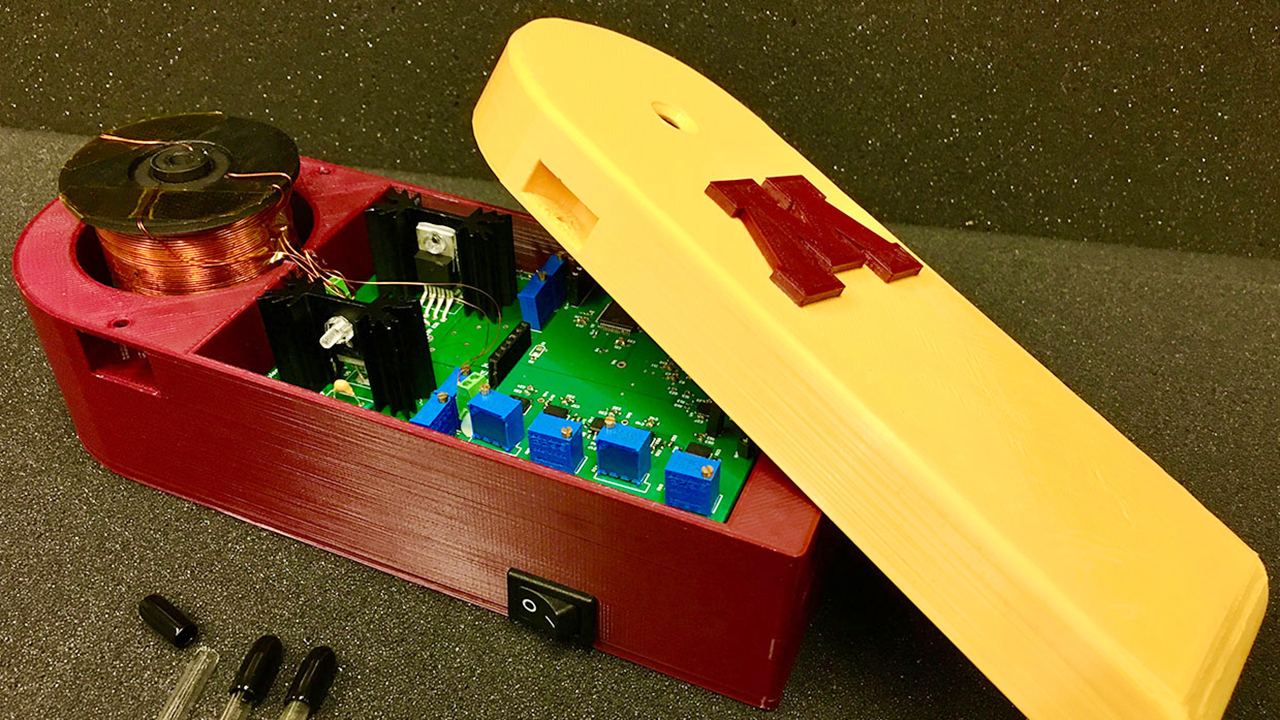
University of Minnesota scientists have designed a portable, low-cost handheld device to detect SARS-CoV-2—the virus that causes COVID-19—in blood and respiratory material and deliver results in as little as 10 minutes.
Through a smartphone interface, the technology platform—called MagiCoil—can also send test results to health professionals, hospitals, and government agencies, allowing for more timely decisions about the care of individuals and providing up-to-date epidemiological data. That will make it easier to monitor the incidence and spread of the virus, which in turn will improve the speed and efficacy of efforts to control the virus while lowering their cost.
Two professors lead the research team. Jian-Ping Wang, PhD, Robert F. Hartmann Chair and Distinguished McKnight University Professor in electrical and computer engineering in the College of Science and Engineering, has worked on the MagiCoil technology platform for 10 years. Maxim Cheeran, PhD, associate professor of veterinary population medicine in the College of Veterinary Medicine, focuses on immunology of viral infections and brain injury.
MagiCoil is based on magnetic particle spectroscopy, or MPS, technology.
“We have been working with Professor Wang and his team, and [with this technology] we have previously demonstrated its ability to detect viruses like H1N1 influenza virus,” Cheeran said.
The MagiCoil starts with a tube containing tiny, magnetic iron oxide nanoparticles suspended in fluid. The nanoparticles have been coated with molecules of, for example, antibodies that recognize and stick to pieces of protein unique to the SARS-CoV-2 virus.
The test involves adding a sample of blood or respiratory material, along with chemicals that break any virus particles apart. This treatment releases the viral proteins and genetic material (RNA) and renders these viral “targets” accessible to the antibodies. The device then applies a magnetic field to the tube.
One part of each viral protein present will stick to a particular antibody on the nanoparticle surface, while another part will dangle freely. The dangling part may stick to a different antibody on another nanoparticle, turning the protein into a bridge holding the two nanoparticles together. As this process repeats, clumps of nanoparticles will form and the magnetic signals coming from the tube will weaken, indicating a positive test result.
Similarly, researchers may build strips of RNA designed to stick to various parts of the viral RNA molecule. Including them, along with antibodies, in the nanoparticle coating will improve the chances of detecting the virus.
“Once our first-generation prototypes are demonstrated successfully, we can ask for a company to produce the device in mass production,” Wang said. “I think there is a way to produce a large enough number of MPS systems to fill a significant portion of the demand.”
The team is now optimizing the device’s design, after which they will move on to three to five months of clinical trials to test it. Once finished, the researchers will work with Minnesota companies to mass-produce the MPS devices at a projected cost of about $100 per unit. The early devices will require professionals to prepare the blood or respiratory samples for testing, but fully automatic devices could follow.
The MagiCoil project is a multidisciplinary effort, drawing on the work of postdoctoral researchers—notably Kai Wu and Venkant Krishna—as well as graduate and undergraduate researchers in the fields of computer science, mechanical engineering, chemical engineering and materials science, and electrical engineering, all working in concert to build up the platform. The project was supported by the UMN Twin Cities’ Medical School and Institute for Engineering in Medicine.
Learn more about the approach on the project's webpage.
This story is based on an article originally published by the College of Science & Engineering.