Nothing about diagnosing and treating a medical condition in the brain sounds simple. Even so, Alik Widge knows that some neurological diseases are more straightforward than others.
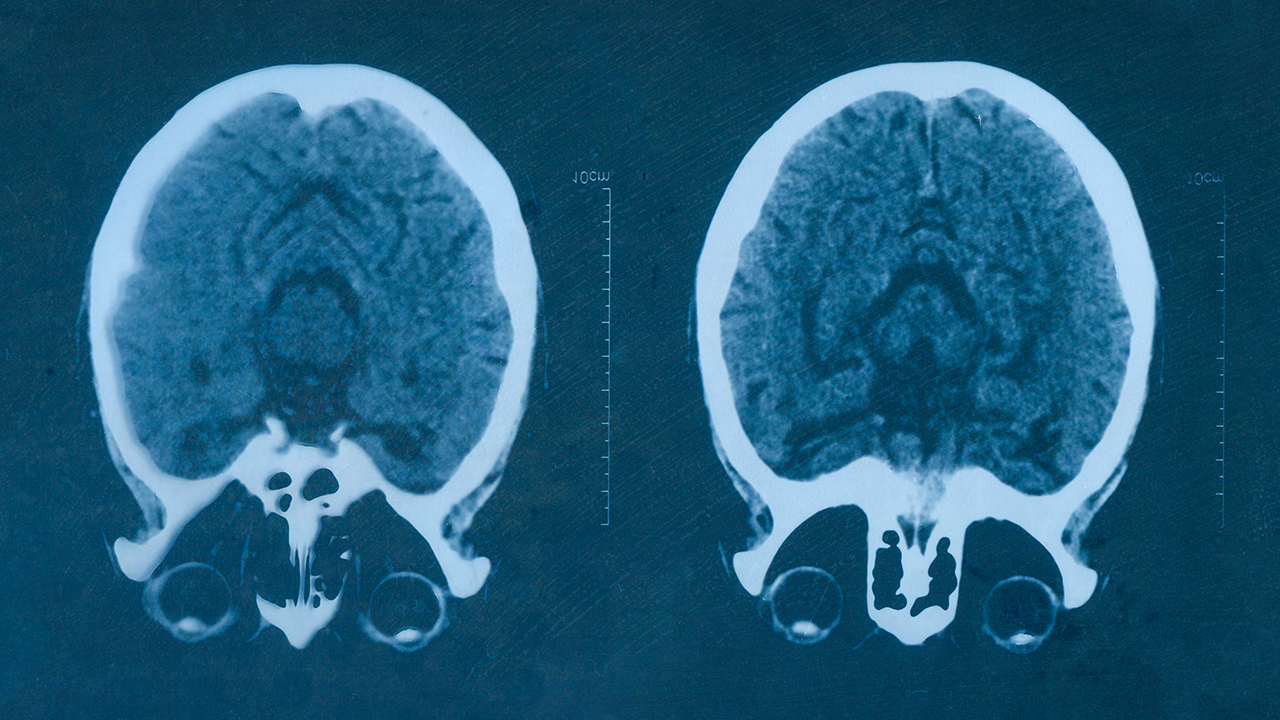
“If you take someone who’s had a stroke and you put them in an MRI scan, you can see there’s a spot in their brain that looks abnormal; that’s where the problem is,” said Widge, MD, PhD, assistant professor of psychiatry in the University of Minnesota Medical School, MnDRIVE neuromodulation scholar, and member of the University's Medical Discovery Team on Addiction. “But if you do that for someone with depression, the brain looks just like everybody else’s. What’s happening is not that the brain is physically abnormal, it’s that something is going wrong in the computations—in the way that individual parts of the brain pass information.”
It’s depression, and a host of other mental health disorders, that Widge and his research team aim to treat more effectively. The team recently received a five-year, $6.6 million grant from the National Institute of Mental Health (part of the National Institutes of Health) to design an implantable medical device that treats psychiatric disorders by adjusting the patterns of activity in certain brain circuits. If successful, the device could provide a new treatment option for conditions like post-traumatic stress disorder, addiction, anxiety, and more.
In addition to Widge, the project’s leaders include Gregory Molnar, PhD, associate professor of neurosurgery in the UMN Medical School and an expert in medical device development and Mahsa Shoaran, PhD, assistant professor at the Swiss Federal Institute of Technology in Lausanne (EPFL) and an expert in signal processing circuits for brain implants.
Syncing Up
The project will build off of existing treatments that rely on a small, surgically implanted wire to deliver electrical pulses to specific parts of the brain. MnDRIVE researchers have previously used this method, called neuromodulation, to stimulate brain activity in a preset pattern that tones down the symptoms of movement disorders where the brain “misfires” signals to the muscles and creates involuntary movements, like Parkinson’s disease.
Psychiatric disorders are finnicky, however, and do not to respond as well to preset patterns. Widge, who is not only a researcher but a clinician, said the lack of effective neuromodulation treatments for mental health conditions have been a point of frustration for him in his medical practice.
Now, he and his team believe they may have found the key to treating psychiatric disorders better. While neural circuits often switch on and off independently during normal brain activity, neighboring parts of the brain sometime line up this activity and start switching on and off in tandem.
“If you look at these waves across regions, sometimes they get into synchrony,” Widge said. “When that happens, information seems to flow better between brain regions. This synchrony of rising and falling rhythms is a signature, and maybe a mechanism, of the brain communicating.”
That led to the idea that stimulation treatments could be designed specifically to coax nearby brain regions into sync, creating a better flow of information that may, for example, alleviate symptoms of anxiety or depression. In other disorders, treatments could involve the opposite—breaking an unusually strong, synchronized connection that leads to compulsive behaviors like addiction.
Sensing the Pattern
The idea relies on the implanted neurostimulator being able to do something that current neuromodulation devices on the market cannot: to lock stimulation to the rise and fall of ongoing brain waves.
In designing the new device, Widge and his team will need to give it greater functionality and processing power than any neurostimulator on the market right now. Since the treatment does involve a surgical implant, it would be geared toward people whose symptoms no longer improve from medications and other treatments. While it may work in tandem with pharmaceuticals, he hopes it could ultimately replace the need for drugs for those who use it.
If all goes well, the team could develop a version of the device ready for manufacturing in as little as five years, a remarkably fast time frame for a medical device. Leading up to that point, however, the endeavor will likely be expensive, complex, and risky (in the sense it may not work as hoped). These types of barriers may make such a project unappealing to established medical device companies, but they fit the bill for a comprehensive research university supported by a federal grant, Widge said.
“There’s this unique convergence of the University’s clinical strength in neuromodulation, the basic engineering work that we’ve been able to do through MnDRIVE, the more translational pieces of MnDRIVE and its industry relations, and the fact that this is one of our state’s dominant industries,” he said. “It created this really perfect opportunity for us to go to NIH and say that we’ve got a vision we think could change everything—and we happen to be in the one place in the world where this vision could come together without too much friction.”